The success of major federal healthcare initiatives, like the Rural Health Transformation Program, the CMS Digital Health Ecosystem and efforts in the VA to expand Community Care, depend on one foundational element: accurate provider data. This article explores why a reliable provider data system is essential for patient access and operational efficiency, and how a data-first approach is the only path to successful execution.
A historic opportunity is presented by federal initiatives like the Rural Health Transformation Program, especially as states finalize their funding applications and CMS and VA determine go-forward strategies. As leaders prepare for award decisions expected at the end of December, the conversation must shift from vision to execution. The success of these programs—along with parallel efforts within the Military Health System—is built upon a crucial, foundational element: the bedrock of accurate provider data.
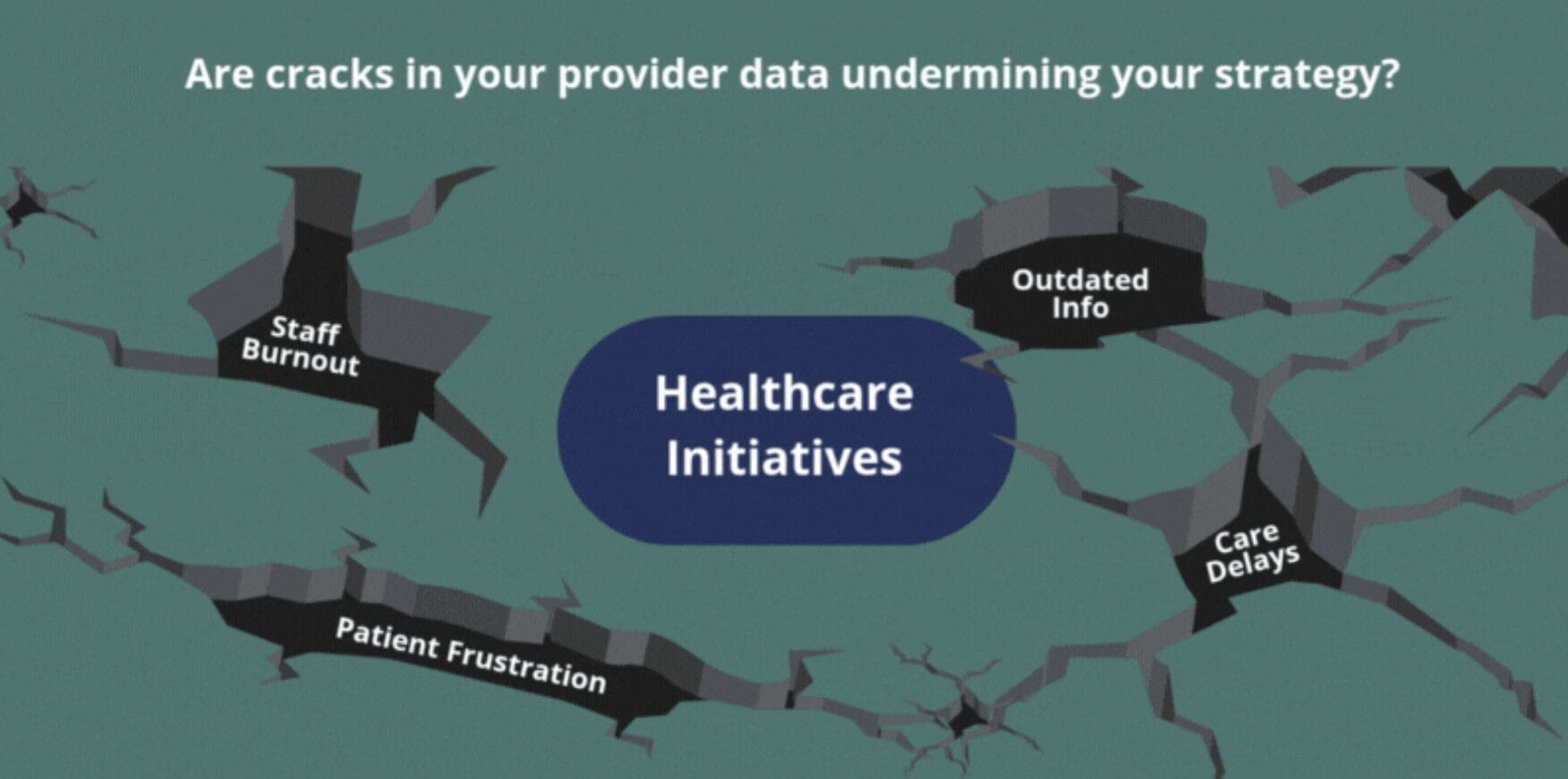
Without a reliable system for understanding who provides what care, where, and when, even the most ambitious and well-funded programs are built on shaky ground. Finding and connecting a person to the right care is the foundation. Without it, every other downstream improvement—from patient engagement and operational efficiency to care management and revenue cycle optimization—becomes meaningless.
The Cracks in the Foundation: Why Bad Data Undermines Policy
The healthcare ecosystem is complex, with provider data often fragmented and siloed across multiple systems, including EHRs, credentialing platforms, and spreadsheets. This leads to a number of costly challenges that directly undermine federal initiatives:
- Undermining Patient Access: Inaccurate or outdated provider information leads to frustrated patients and care delays. A patient searching for an in-network, in-person appointment for a specific condition may find a listing that is out-of-date, for a provider who is no longer accepting new patients, or for an office that is miles away from where they live. This directly obstructs the goals of improving access, especially for rural residents and veterans who already face the challenge of finding care among fewer local options.
- Operational Inefficiencies: For health systems, managing this data manually is a significant drain on resources. For smaller group and rural practices, this manual data management is nearly impossible, contributing to the administrative burnout that initiatives like the RHTP aim to alleviate. Staff members are often tasked with correcting billing errors, verifying provider information, and navigating fragmented systems, taking their focus away from higher-value work. For an enormous integrated health system like the Veterans Health Administration, cobbling together interfaces and unproven solutions to manage provider data is a recipe for disaster.
- Failed Strategic Partnerships: Fostering strategic partnerships (Goal 2 of the CMS Rural Health Transformation) is difficult when provider networks and capabilities are not accurately and centrally mapped. Without a “single source of truth” for provider data, it is nearly impossible for organizations to collaborate effectively, share best practices, or optimize capacity utilization.
The Blueprint for a Strong Foundation: A Data-First Approach
Large-scale public sector healthcare initiatives can only succeed if they prioritize a data-driven approach to provider management. This means investing in a centralized provider data management strategy that unifies disparate information into a single, accurate source that is actively curated and maintained over time by a strategic partner experienced in this work at scale.
For example, the Veterans Health Administration is seeking to replace their outdated PPMS system with a modern Provider Directory for their Community Care Network. This vital care for our nation’s Veterans should not depend on an immature solution not proven at scale. That is why Kyruus Health is teaming with Salesforce and others to propose a proven provider data management solution that can be delivered at scale on a trusted and low-cost FedRAMP High authorized platform.
Kyruus Health’s solution highlights how this foundation is essential for powering enterprise-wide initiatives for patients, providers, and payers. Boiled down to their essence, all the current strategic initiatives in federal health seek to accomplish three key objectives:
- Improve Access: Technology powered by accurate data can guide patients to the best-suited provider based on their clinical needs and personal preferences, reducing the number of people who skip or delay care because they cannot find an appropriate appointment.
- Enhance Financial Viability: Accurate data helps streamline the revenue cycle and reduce administrative costs, directly supporting the financial solvency of rural hospitals and other providers.
- Optimize Care Delivery: A comprehensive view of the provider base helps clinical and administrative staff better manage care transitions and ensures clinicians are practicing at the top of their licenses, leading to more efficient and higher-quality care.
As we work with our Federal health partners to create a more effective and accessible healthcare system, the path forward is clear. Grand visions for transformation, like the Rural Health Transformation Program, set the destination. But the journey there is paved with data.
With funding applications and procurements underway, the focus now shifts to making these ambitious plans a reality. As states and agencies anticipate award decisions at the end of this year, it is the perfect time to solidify the data strategy that will underpin their programs. The success of these vital initiatives hinges on a fundamental shift in perspective: we must recognize that accurate provider data is not a logistical afterthought, but the very bedrock upon which all other improvements are built.