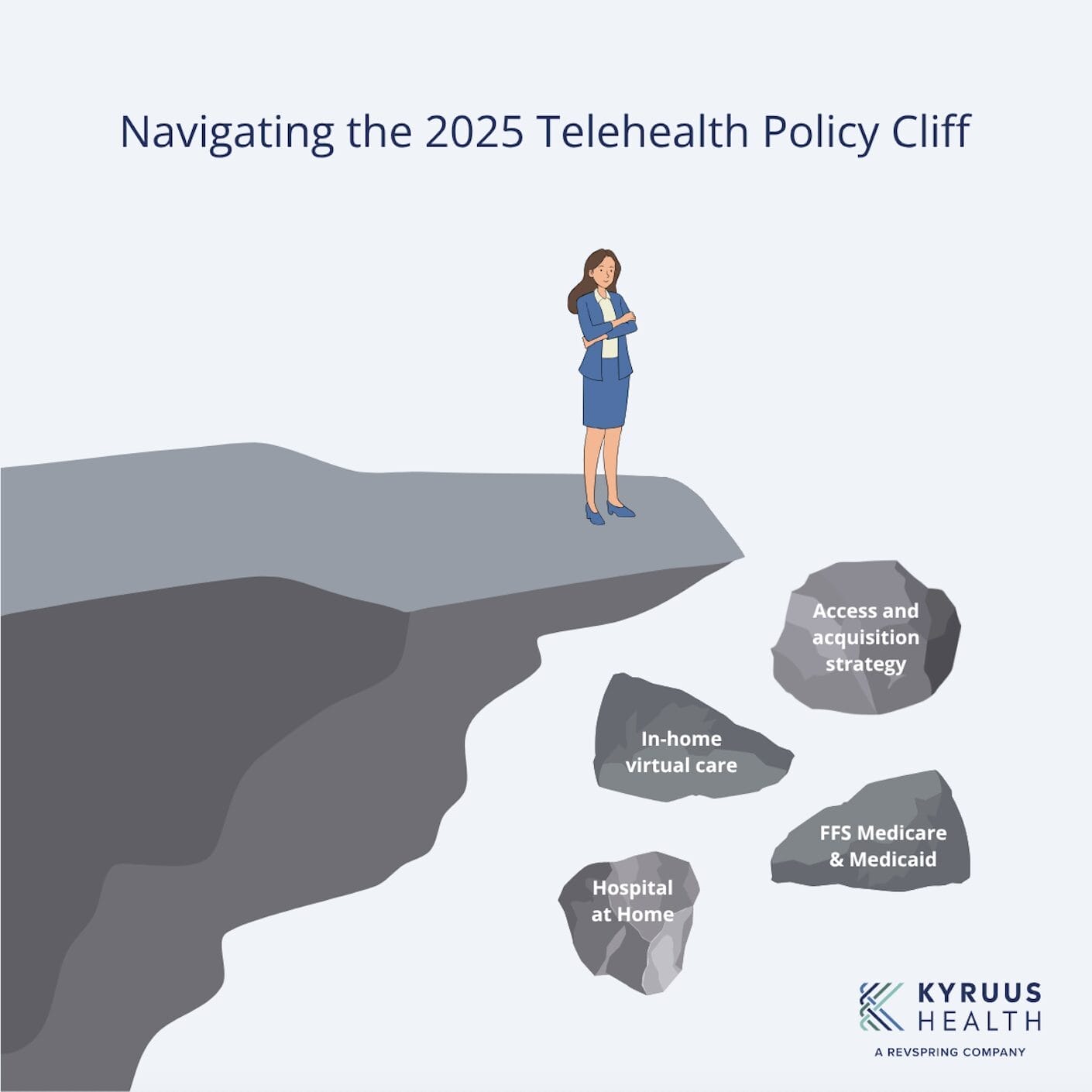
The date has passed. For over a year, health systems across the United States looked to September 30, 2025, with a mix of hope and anxiety. We hoped Congress would act to make the pandemic-era telehealth flexibilities permanent. Instead, the anxiety won. The Telehealth Policy Cliff is no longer a future problem; it is today’s operational crisis.
The expiration of key reimbursement flexibilities, especially for in-home care and Fee-for-Service (FFS) Medicare and Medicaid, has thrown a wrench into the most innovative care models deployed in the last five years. Programs like Hospital at Home (HaH), which were celebrated for improving patient outcomes and freeing up hospital capacity, are now on financially unstable ground.
Health systems are being forced to re-evaluate their financial risk from the top down. Can we continue to offer in-home virtual care? What happens to our patient acquisition and access strategies, which are now heavily reliant on these modalities?
But this isn’t just a financial or policy problem. It’s an operational and human-centric one. It exposes the deep, fragmented cracks in our healthcare infrastructure and reinforces the urgent, non-negotiable need for a unified platform to manage provider data, streamline care routing, and automate processes. This is no longer about innovating for the future; it’s about surviving the present.
What is the 2025 Telehealth Policy Cliff, and What Exactly Did It Change?
The 2025 Telehealth Policy Cliff is the term used to describe the operational crisis resulting from the expiration of key federal reimbursement flexibilities that supported virtual and in-home care models. Health systems had hoped Congress would make these pandemic-era flexibilities—which ceased on September 30, 2025—permanent. Their expiration has destabilized innovative care models like Hospital at Home (HaH).
The temporary federal waivers had temporarily removed decades-old barriers to telehealth. With those waivers now gone, the healthcare landscape has reverted, creating two massive operational hurdles for health systems:
- Reimbursement Uncertainty: Guarantees that FFS Medicare and Medicaid would reimburse for a wide array of in-home telehealth services have vanished. Every virtual visit offered to this population outside of a traditional clinic setting is now a potential financial liability.
- Geographic & Modality Restrictions: Strict, pre-pandemic rules are back in force. These rules govern where a patient must be located (e.g., qualifying rural area) and what type of provider and modality (e.g., video vs. audio-only) is eligible for reimbursement.
This reversion forces health systems to either roll back popular in-home virtual care options or absorb unsustainable financial risk.
What is the Downstream Impact of This Policy Change on Staff and Patients?
The immediate, negative impact of the Telehealth Policy Cliff is felt by a health system’s two most valuable assets: its workforce and its patients. This operational chaos significantly increases administrative burden, fuels clinical burnout, and leads to widespread patient confusion.
Impact on Workforce (Burnout & Inefficiency)
Front-line staff—including care coordinators, schedulers, and clinical staff—are now tasked with navigating a confusing maze of conflicting eligibility rules. This leads to:
- Increased Manual Work: Staff must spend excessive time determining which provider, in which location, offering which specific modality, is actually reimbursable for a specific patient under the new rules.
- Patient Dissatisfaction: Staff must deliver frustrating news, such as “I’m sorry, you must now come into the office for a visit you had at home last month.”
- Burnout and Turnover: This increased administrative load and constant need to manage patient complaints are soul-crushing factors that drive clinical burnout and staff turnover.
Impact on Patient Access
The fragmentation is magnified for large, dispersed health systems. Without a central system, managing provider data, licensure, and availability across multiple regions with differing policy rules becomes impossible, resulting in a fractured and frustrating patient experience.
How Can Health Systems Mitigate the Financial and Operational Risk?
Health systems cannot change Congressional policy, but they can and must change their operations by deploying a resilient, unified care access platform. The wrong response is to attempt management via spreadsheets, internal memos, or manual overrides in the EHR; this is a recipe for revenue denial and staff attrition.
A robust care access platform creates a single, unified source of truth for provider and location data that automates eligibility checks and guides patients through scheduling the right, reimbursable care.
A platform approach, such as that offered by Kyruus Health, directly solves the crisis of the Telehealth Policy Cliff in three key areas:
1. Unify Your Provider Data (The “Who”)
Question: Who is eligible to perform this virtual visit under the new rules?
- The Solution: The platform unifies all disparate provider and location data (from EHRs, credentialing, etc.) into one clean, accurate record.
- Key Function: This central record tracks critical eligibility data, including current licensure, specialties, and the specific virtual services they are cleared to offer under the new policy rules. When policy changes occur, only one central record needs updating.
2. Streamline Care Routing (The “Where”)
Question: How do we get the patient to the right setting that is financially viable for the system?
- The Solution: Advanced search and scheduling solutions leverage this unified data to automatically route patients.
- Key Function: The platform automatically filters and presents patients (or call center agents) with options that are clinically appropriate, available, and, most importantly, financially viable for the health system. This prevents out-of-policy bookings before they happen.
3. Automate Financial and Administrative Processes (The “How”)
Question: How do we ensure efficiency and protect the revenue cycle from denials?
- The Solution: The platform automates pre-visit administrative and financial checks.
- Key Function: By automating the check-in and pre-visit process, the system can validate eligibility and surface cost estimates. This strips away the manual search and verification work that burns out staff, ensuring providers see the right patients and protecting the revenue cycle from a flood of claim denials.
Don’t Let the Telehealth Policy Cliff Define Your Future
The Telehealth Policy Cliff is a disruptive event, but it serves as a “burning platform” moment—an urgent opportunity to finally address the fragmented systems and inaccurate data that have plagued healthcare for decades.
By implementing a robust care access platform, you create critical connections across your entire healthcare ecosystem, empowering your stressed workforce and ensuring you can continue your mission: to connect people to the right care, no matter how complex the policy landscape becomes.
As the industry’s largest care access platform, Kyruus Health, a Revspring company, empowers healthcare organizations to manage their data, automate their workflows, and build a more resilient, friction-free experience for everyone.