The healthcare industry is undergoing a period of rapid transformation, with new regulations and executive orders reshaping the landscape for health plans. These changes, while aimed at improving the healthcare system, also present challenges for health plans as they strive to maintain compliance and deliver exceptional member experiences.
This article focuses on recent executive orders and proposals, outlining key strategic considerations for health plans to navigate these changes while prioritizing a member-first approach.
Key Executive Orders and Proposals
Health plans today are challenged to keep up with the pace of regulatory change, such as some of the recent updates and proposals that we’re keeping a close eye on:
- Promoting Competition and Transparency in Healthcare: Executive orders and proposals aimed at increasing transparency in the healthcare industry have emerged, with a focus on empowering consumers with clear and accessible information about costs, provider networks, and quality of care. These initiatives could have significant implications for health plan operations, particularly in areas such as cost estimation tools, provider directories, network design, pricing strategies and member engagement.
- Enhancing Medicare and Medicaid Programs: Proposals to strengthen Medicare and Medicaid programs have been put forth, including expanding benefits, improving access to care, and addressing health equity. These proposals could impact health plan operations by influencing benefit design, provider networks, and care delivery models.
- Strengthening Mental Health Parity: Proposals to enforce mental health parity laws and improve access to mental health services have been introduced. This could impact health plan benefit design, provider networks, and utilization management practices.
- Curbing Improper Enrollments in the Marketplaces: As we see it, this administration is making quick changes, with the CMS recently proposing new rules to focus on improper enrolments through ACA plans. This is likely the first of many new considerations expected this year.
Strategic Considerations for a Member-First Approach
- Transparency and Communication: Increased transparency is a recurring theme in recent regulations. Health plans need to proactively communicate with members about changes to benefits, costs, and network composition. Clear, concise, and accessible information is crucial to empower members to make informed decisions about their care.
- Access to Care: Network adequacy and timely access to care are key concerns. Health plans need to ensure their networks provide sufficient access to a diverse range of providers, including specialists and mental health professionals. Leveraging technology to streamline appointment scheduling and reduce wait times can further improve access.
- Data Management and Privacy: Accurate provider data is crucial for compliance with transparency regulations and for member decision-making. Health plans need to invest in robust data management solutions to ensure data accuracy and protect member privacy.
- Member Engagement: Actively engage members in their healthcare journey through personalized communication, digital tools, and support programs. Understand member needs and preferences to tailor services and improve satisfaction.
- Value-Based Care Alignment: As the industry shifts towards value-based care, health plans need to align their strategies with this model. This includes partnering with providers to improve quality, outcomes, and cost-efficiency of care.
How Kyruus Health Can Support a Member-First Approach
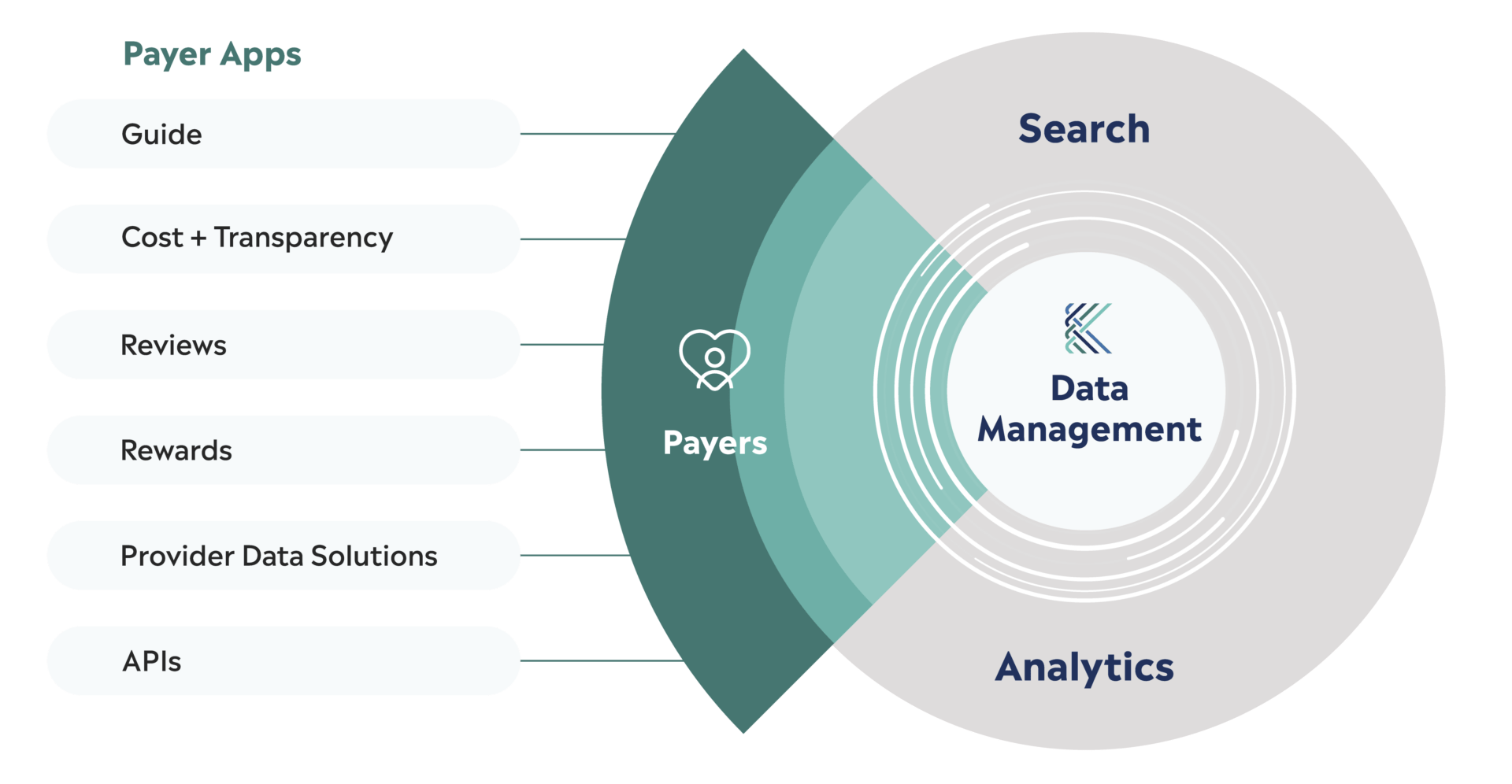
Kyruus Health offers a suite of solutions designed to help health plans navigate these challenges and deliver exceptional member experiences:
- Provider Data Solutions: Ensure accurate and up-to-date provider data to power transparency initiatives, member decision-making, and network optimization.
- Care Access and Navigation: Empower members to find the right providers, schedule appointments easily, and access care seamlessly.
- Advanced Analytics: Gain insights into member behavior, network performance, and cost drivers to inform strategic decision-making and improve outcomes.
By embracing a member-first approach and leveraging innovative solutions, health plans can successfully navigate the changing regulatory landscape and continue to provide high-quality, accessible care to their members.



