Provider Data Management: A Key to Health Plan Financial Health
Capturing and maintaining accurate provider data is a critical component of a health plan’s success, yet one that remains a top challenge. Despite regulations aimed at improving the reliability of physician directories, a staggering 81% of entries still exhibit inconsistencies, as highlighted by a study in the Journal of the American Medical Association. Provider information is frequently changing, making the task of maintaining this dynamic data seem daunting. Additionally, data is often fragmented, presenting a continuous challenge in pinpointing and correcting inaccuracies. To effectively tackle these challenges, health plans must not only ensure their data is accurate, but create a strong foundation with a centralized data repository that ensures uniformity across all channels.
Five Key Areas Impacting Bottom Line
This guide explores the various provider data obstacles faced by health plans and presents a compelling business case for robust provider data management, emphasizing its vital role in five key areas with direct impact on health plans’ bottom line:
- Member experience: driving member growth and retention
- Access to care: reducing out-of-network claims
- Regulatory compliance: reducing the risk of regulatory penalties
- Provider network collaboration: streamlining provider profile enhancements
- Improving operational efficiency: reducing manual data updates
Member Experience: Driving Member Growth and Retention
Members first turn to their health plan when searching for care online, expecting a straightforward and efficient process. Unfortunately, reality often falls short of these expectations. With outdated or incorrect information and lack of essential provider details, including languages spoken, years in practice, and treatment philosophy, members are having a hard time finding providers that truly meet their needs. A recent survey reveals that a significant majority of members are not only seeking more accurate information but also demanding more detailed provider profiles. With accurate and robust information, members can navigate their healthcare options more effectively, remain within their network, and confidently choose the care that best suits their needs.
- 62% of members want more accurate information from their health plans.
- 70% of Millennials and 64% of Gen Z members wish their health plan provided more detailed provider profiles.
- 114% increase in member interactions with enhanced compared to non- enhanced provider profiles.
MAKING THE BUSINESS CASE: MEMBER GROWTH AND RETENTION
Enhancing the quality of data that informs member interactions strengthens the trust and engagement between members and their health plan. This engagement, in turn, leads to higher membership acquisition and retention rates. Membership growth is a vital driver of health plan financial success, with gross margin per enrollee (in the group and individual markets) exceeding $900 in 2023.
Access to Care: Reducing Out-of-Network Claims
Insufficient and unactionable provider data significantly hinders access to care and increases the total cost of care. This is largely due to incomplete information that creates barriers, inaccurate information that complicates the search process, and lack of online scheduling capabilities that are only possible with reliable provider data. When members struggle to find the care they need, they are far more likely to postpone or forego care altogether. In the past year, one-third of members encountered incorrect provider information on health plan digital platforms, and 30 percent of these members chose to skip care as a result. Missed annual wellness checks and preventive screenings are the most frequent types of neglected care, leading to higher overall costs due to delayed diagnoses, increased emergency visits, and other complications.2 Additionally, poor data quality contributes to the prevalence of âghost networks,â where members are mistakenly directed to out-of-network providers, disrupting ongoing care and generating extra costs for both members and health plans.
- 18% of inpatient admissions and 8 percent of outpatient services involve an out-of-network provider claim, each adding an average of $350 in costs per encounter.
- 70% of members with unaffordable out-of-network medical bills were unaware that their provider was out of network until after receiving care.
Types of Care Consumers Are Delaying or Skipping
What type(s) of medical care did you delay or skip? (Asked among those who have delayed and/or completely skipped receiving any kind of medical care in the past year)

Click to enlarge
Enhancing Healthcare Access through Online Appointment Scheduling
In today’s digital era, providing online scheduling capabilities is crucial for improving access to care and meeting member expectations. However, despite 80 percent of members expressing a preference to book appointments via their health plan’s website, more than half have foregone care because they couldn’t schedule their appointments online. Integrated appointment scheduling enables members to easily locate and access in-network care with providers that meet their needs.
MAKING THE BUSINESS CASE: REDUCING OUT-OF-NETWORK CLAIMS
Nearly 18 percent of inpatient admissions and 8 percent of outpatient services involve an out-of-network provider claim, each adding an average of $350 in costs per encounter.Alarmingly, about 70 percent of members with unaffordable out-of-network medical bills were unaware that their provider was out of network until after receiving care. This underscores the critical need for health plans to provide clear and accurate provider information. By investing in reliable and actionable provider data, health plans can drastically reduce these out-of-network occurrences. Improved data quality not only ensures that members receive accurate and comprehensive information, but also streamlines the process of scheduling in-network appointments. Such enhancements in data management are also likely to decrease the number of members who delay or forgo care due to the challenges of navigating their health plan’s network, ultimately fostering better health outcomes and member satisfaction.
Regulatory Compliance: Reducing the Risk of Penalties
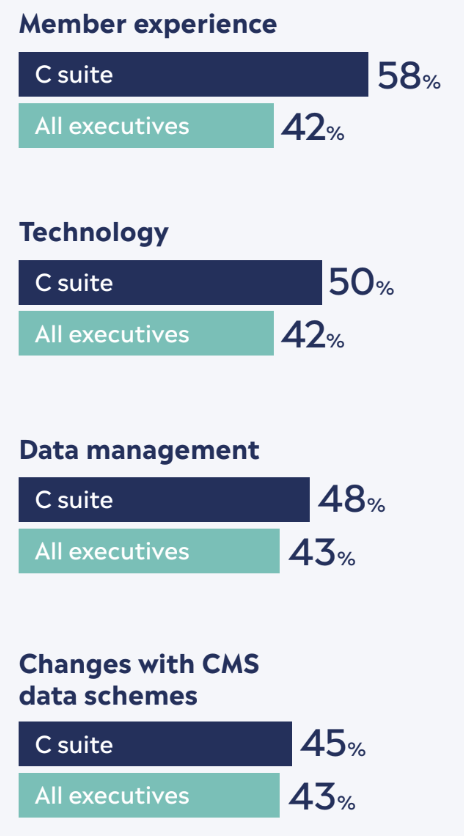
In recent years, regulatory mandates have been introduced to tackle poor data quality. Maintaining accurate provider data is crucial, as inaccuracies can compromise member experiences and lead to significant penalties. Under the No Surprises Act, health plans must verify the accuracy of their provider data quarterly and update any discrepancies within two days. Additionally, with the introduction of the proposed REAL Health Providers Act, which aims to eliminate ghost networks, health plans must remove providers no longer in-network within five business days. While compliance is vital, the effectiveness of the updated information hinges on how comprehensively it is presented to members. A majority of C-level health plan executives view enhancing member experience as a significant challenge in complying with transparency mandates.
For example, although health plans are mandated to publish machine-readable files with negotiated rates, this data often lacks context and includes billing codes that are meaningless to members. Therefore, it is essential for health plans to extend their efforts beyond compliance. They need to ensure that the data is not only accurate but also accessible and understandable to members, thereby making a real impact rather than just fulfilling a regulatory requirement.
Plan executives cite key challenges in keeping up with price transparency mandates
Click to enlarge
MAKING THE BUSINESS CASE: REDUCED RISK OF A PENALTY
Data compliance drives return on investment for health plans by reducing risks associated with external risk assessments, regulatory fines, and legal liabilities. Robust compliance protocols minimize the likelihood of financial repercussions while fostering trust among members.
Provider Network Collaboration: Streamlining Provider Profile Enhancements
Effective collaboration between providers and health plans is essential for maintaining accurate directories. Providers depend on health plan portals to update their information, yet they often encounter challenges like inconsistent submission requirements and a cumbersome process. Consequently, only 20 percent of providers are confident that directories accurately and comprehensively represent their facilities and staff. Despite these obstacles, the need for improved directory data is widely acknowledged, with 97 percent of hospitals and health plans recognizing its importance, according to a recent survey. The stakes are high, as poor digital experiences can drive consumers away-Â over a third of healthcare consumers are willing to switch providers for the convenience of online appointment booking.
Only 20% of providers are confident that directories accurately and comprehensively represent their facilities and staff.
MAKING THE BUSINESS CASE: STREAMLINING PROVIDER PROFILE ENHANCEMENTS
By investing in solutions that enable providers to easily supply information, health plans can significantly enhance the accuracy of the data collected. Building strong provider relationships from the outset ensures a smoother data collection process, leading to more reliable and verified information. Additionally, establishing a centralized data repository creates consistency across channels when these updates are made. These approaches streamline data maintenance and reduce labor costs associated with data management.
Operational Efficiency: Reducing Manual Data Updates
The daily operations involved in managing data can put a significant drain on resources. By tackling the root causes of inefficient data management and implementing a system that guarantees data synchronization, health plans can ensure that updates are accurately reflected in all areas, effectively preventing any potential downstream problems.
A sophisticated provider data management solution- and governance process – automates tasks and workflows, saving time and costs, and sidestepping challenges associated with developing solutions in-house.
Accuracy of data across digital channels is a must for health plans, but it is also important to note that members who are not utilizing health plan digital tools are often turning to providers or customer service for information. By deploying a provider data management solution that offers real-time updates across all touchpoints, everyone from call center agents to care navigators are consistently equipped with up-to-date provider information, ensuring a seamless flow of accurate information and enhancing overall operational efficiency.
- 42% of members get their healthcare information from customer service
- 32% of members get their healthcare information from their provider
MAKING THE BUSINESS CASE: REDUCING MANUAL DATA UPDATES
Collecting, validating, and maintaining accurate provider information is an expensive and labor-intensive process. Streamlining these processes can alleviate the administrative burdens tied to data management, such as time and labor costs involved in manual updates. Improving data accuracy will also encourage the adoption of digital solutions, allowing more members to manage their tasks online and further reducing administrative overhead. Additionally, for members who still prefer traditional support channels, health plans can enhance efficiency by ensuring that customer service representatives have access to reliable information, enabling them to assist members quickly and effectively.
Top Strategies for Effective Provider Data Management
Effective management of provider data is critical for the operational success of health plans, significantly impacting member retention, health outcomes, and compliance with regulations. To build a more responsive, efficient, and member-centric system, health plans can consider the following strategies:
- Establish a centralized data repository to maintain uniformity and accuracy across all channels.
- Revamp provider directories with comprehensive, up- to-date information to increase member trust and satisfaction.
- Integrate online scheduling functionality that allow members to easily book appointments, improving access to care.
- Establish regular verification processes to ensure provider information is current and compliant, minimizing penalty risks.
- Provide tools for providers to update their own information, ensuring data accuracy and reducing administrative burdens.
- Implement advanced technologies to automate data management, enhancing efficiency and reducing costs.
Ready to take the next step?
Learn how Kyruus Health’s provider data management solutions can drive
measurable return on investment for your organization. Contact us today to
request a free ROI analysis customized for your health plan.



