The healthcare industry is rapidly evolving, and with it, the complexity of managing provider data has grown immensely. For health plans, the accuracy and consistency of provider information directly impacts member experience, access to care, regulatory compliance, provider collaboration, and operational efficiency. Yet, despite the increasing focus on data management, the challenge remains considerable. A staggering 81% of provider directory entries still contain inconsistencies, according to a study published in the Journal of the American Medical Association. This discrepancy not only compromises member satisfaction but also leads to significant financial consequences for health plans.
In this blog, we’ll explore the critical importance of provider data management for health plans, the tangible impact it has on their financial health, and the strategies needed to overcome common challenges. By the end, it will be clear that effective provider data management is not just a regulatory obligation but a powerful tool for improving member experience, reducing costs, and driving sustainable growth.
The Business Impact of Provider Data Management
For health plans, provider data management influences five key areas that directly impact their bottom line:
- Member Experience
- Access to Care
- Regulatory Compliance
- Provider Network Collaboration
- Operational Efficiency
Each of these elements plays a vital role in a health plan’s overall success, and all are dependent on the quality of provider data. Let’s examine how accurate provider data influences each of these factors and how it can drive measurable improvements for health plans.
1. Provider Data Management Enhances Member Experience
 Members look to their health plans for accurate, timely, and detailed information about healthcare providers. When they search for a provider through their health plan’s website, they expect to find up-to-date details on important factors like practice locations, languages spoken, years of experience, and treatment philosophy. Unfortunately, outdated or inaccurate information is a common problem, leading to frustration and dissatisfaction among members.
Members look to their health plans for accurate, timely, and detailed information about healthcare providers. When they search for a provider through their health plan’s website, they expect to find up-to-date details on important factors like practice locations, languages spoken, years of experience, and treatment philosophy. Unfortunately, outdated or inaccurate information is a common problem, leading to frustration and dissatisfaction among members.
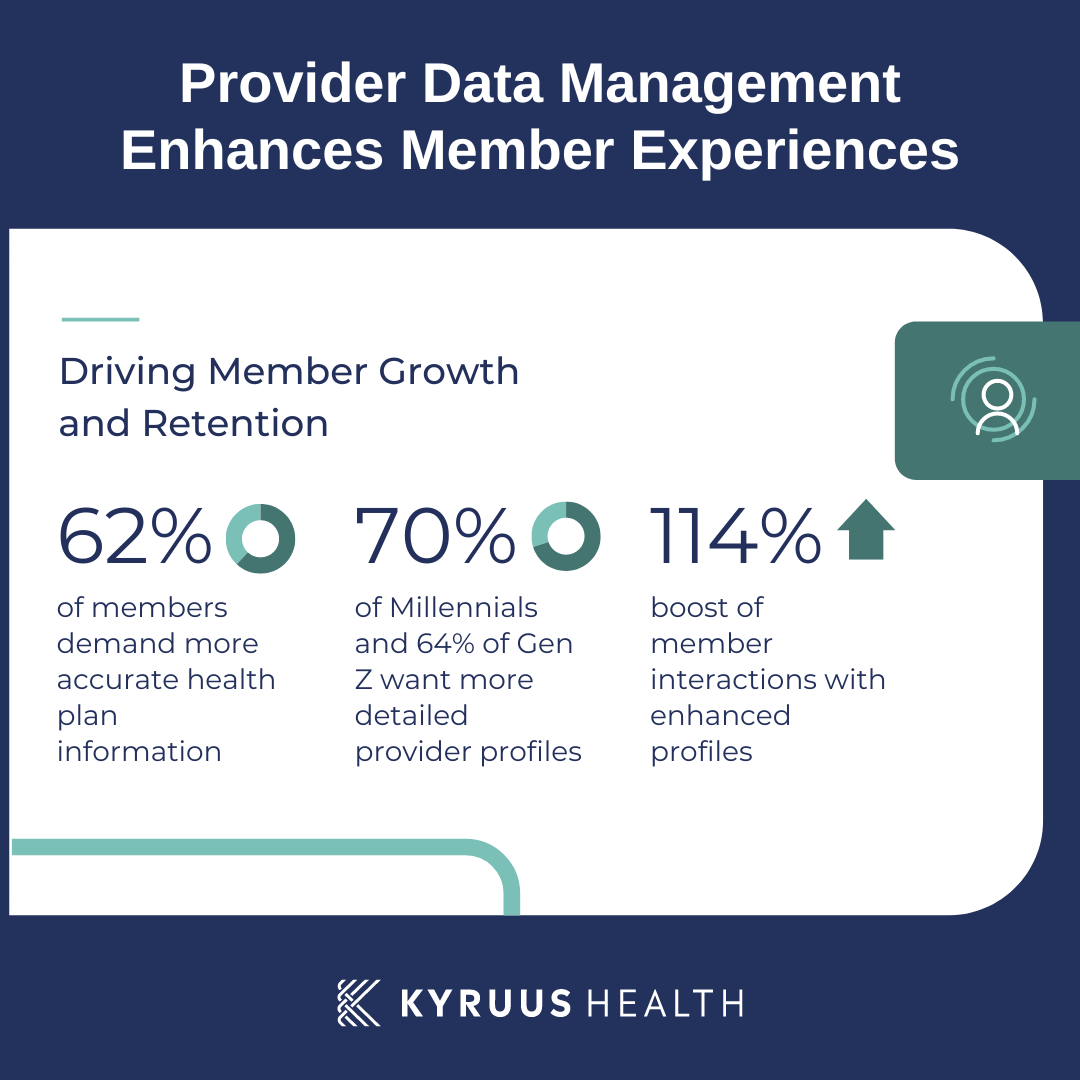
A recent survey revealed that 62% of members want more accurate information from their health plans, and this need is even more pronounced among younger generations. 70% of Millennials and 64% of Gen Z members expressed a desire for more detailed provider profiles.
The consequences of poor provider data are significant: members may leave their health plan, seek care outside their network, or delay care altogether. In contrast, providing accurate and comprehensive information builds trust between members and their health plans, encouraging them to stay within the network and take advantage of the care options available to them. This translates into higher retention rates and increased member satisfaction, both of which are critical for financial success.
For instance, health plans that offer enhanced provider profiles have reported a 114% increase in member interactions compared to those with non-enhanced profiles. This demonstrates the powerful impact that well-managed provider data can have on member engagement.
2. Provider Data Management Improves Access to Care
 Accurate provider data doesn’t just improve member experience—it also plays a critical role in ensuring that members can access in-network care. When provider directories contain outdated or incorrect information, members are more likely to seek care outside of their network, leading to higher out-of-network claims and increased healthcare costs for both the plan and the member.
Accurate provider data doesn’t just improve member experience—it also plays a critical role in ensuring that members can access in-network care. When provider directories contain outdated or incorrect information, members are more likely to seek care outside of their network, leading to higher out-of-network claims and increased healthcare costs for both the plan and the member.
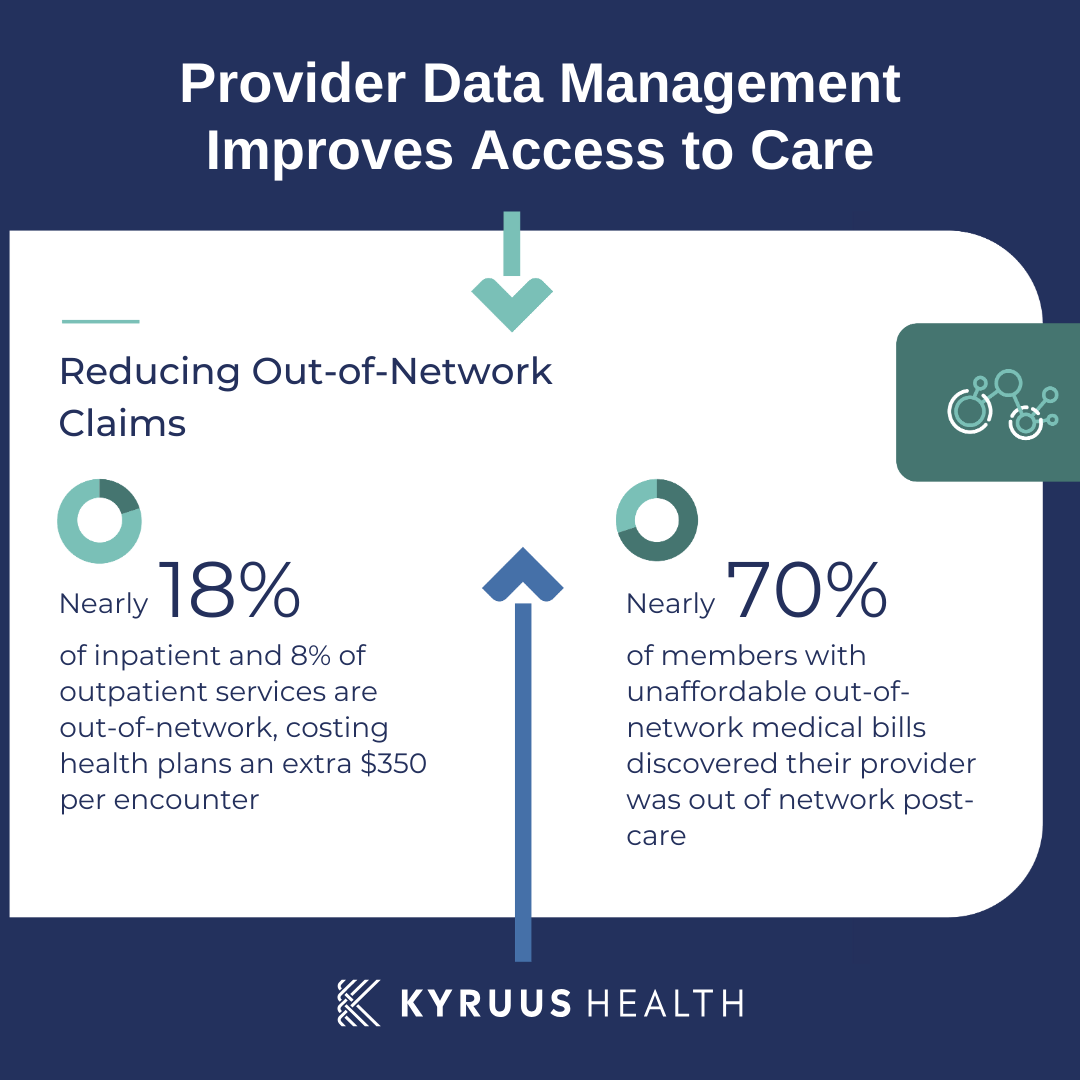
In fact, 18% of inpatient admissions and 8% of outpatient services involve an out-of-network provider claim, each adding an average of $350 in costs per encounter. Even more concerning, 70% of members who faced unaffordable out-of-network medical bills were unaware that their provider was out-of-network until after receiving care.
By investing in accurate, up-to-date provider data, health plans can help members avoid these costly surprises. Additionally, integrating features like online appointment scheduling, which relies on accurate provider data, allows members to easily book in-network care, further reducing the likelihood of out-of-network claims.
3. Provider Data Management Ensures Regulatory Compliance
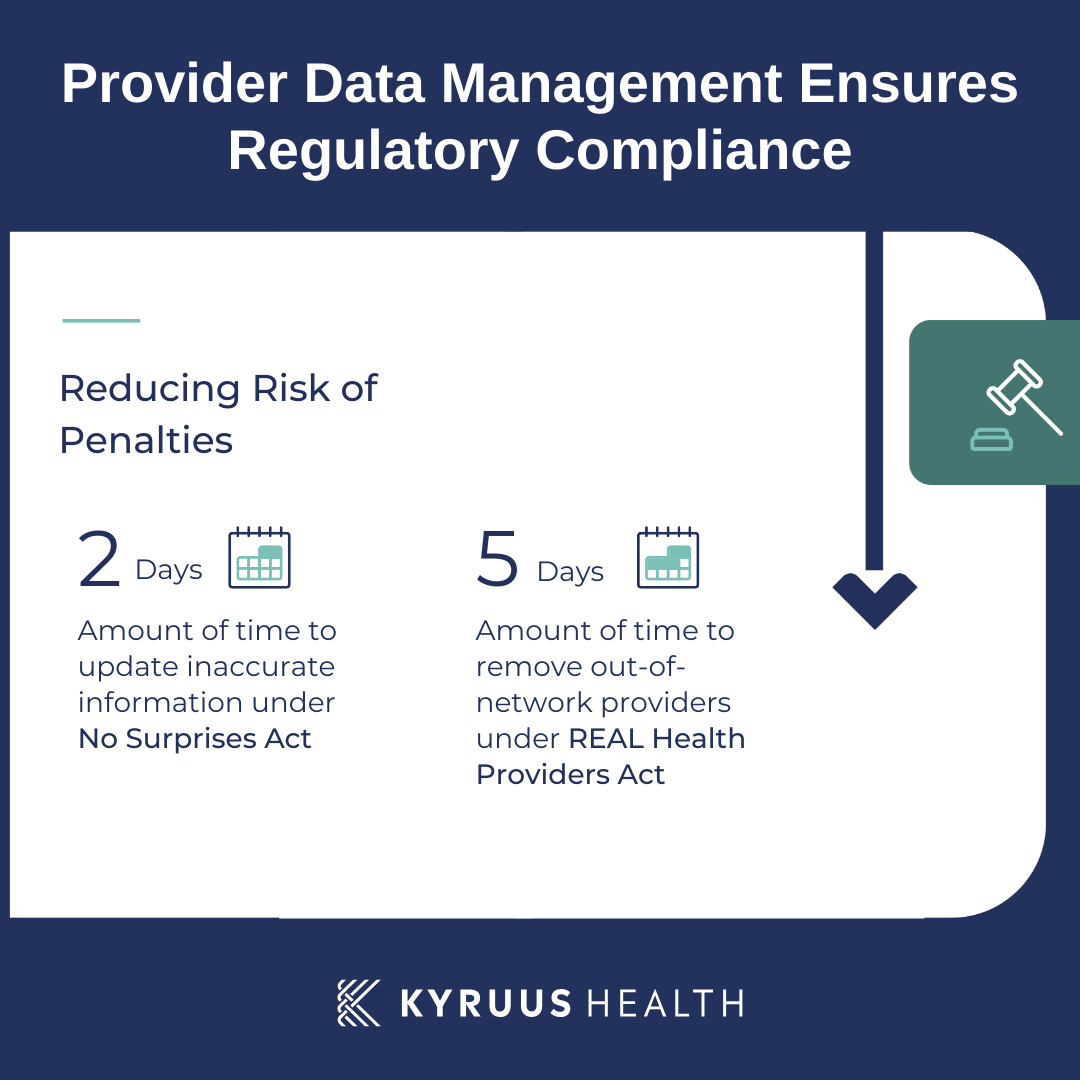 The regulatory landscape surrounding provider data management has become increasingly stringent in recent years. Legislation such as the No Surprises Act and the proposed REAL Health Providers Act requires health plans to verify the accuracy of their provider directories regularly and remove any outdated or incorrect information.
The regulatory landscape surrounding provider data management has become increasingly stringent in recent years. Legislation such as the No Surprises Act and the proposed REAL Health Providers Act requires health plans to verify the accuracy of their provider directories regularly and remove any outdated or incorrect information.
Failure to comply with these regulations can result in significant penalties. For example, health plans must now verify provider data quarterly and correct discrepancies within two days. Under the proposed REAL Health Providers Act, health plans must remove providers who are no longer in-network within five business days. Non-compliance could lead to steep fines and damage the health plan’s reputation.
However, compliance isn’t just about avoiding penalties. Health plans that proactively ensure their provider data is accurate, accessible, and understandable to members are better positioned to build trust and foster positive member experiences. By going beyond the minimum requirements of the law, health plans can differentiate themselves in a competitive marketplace while also reducing their risk of financial penalties.
4. Provider Data Management Improves Provider Network Collaboration
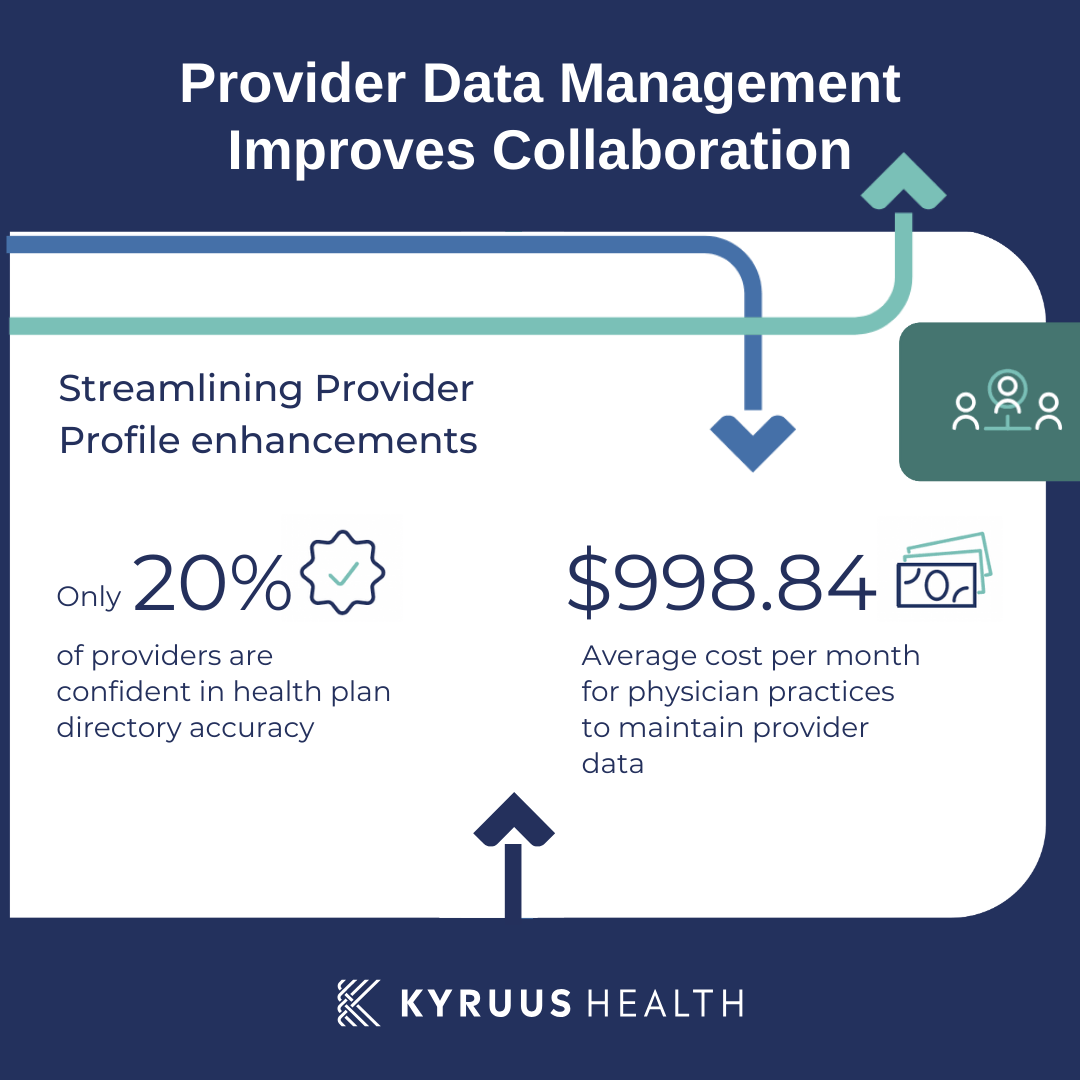 Collaboration between providers and health plans is essential for maintaining accurate provider directories. Providers rely on health plans to ensure their information is represented accurately, but they often encounter challenges like inconsistent submission requirements and cumbersome processes for updating their details. As a result, only 20% of providers feel confident that their health plan directories accurately represent their facilities and staff.
Collaboration between providers and health plans is essential for maintaining accurate provider directories. Providers rely on health plans to ensure their information is represented accurately, but they often encounter challenges like inconsistent submission requirements and cumbersome processes for updating their details. As a result, only 20% of providers feel confident that their health plan directories accurately represent their facilities and staff.
Health plans can improve this situation by streamlining the process for providers to update their own information. Implementing user-friendly tools and systems for providers to submit updates can significantly improve data accuracy and reduce the administrative burden on both providers and the health plan. By investing in these solutions, health plans can foster stronger relationships with their provider networks, leading to more accurate and comprehensive directories.
5. Provider Data Management Leads to Operational Efficiency
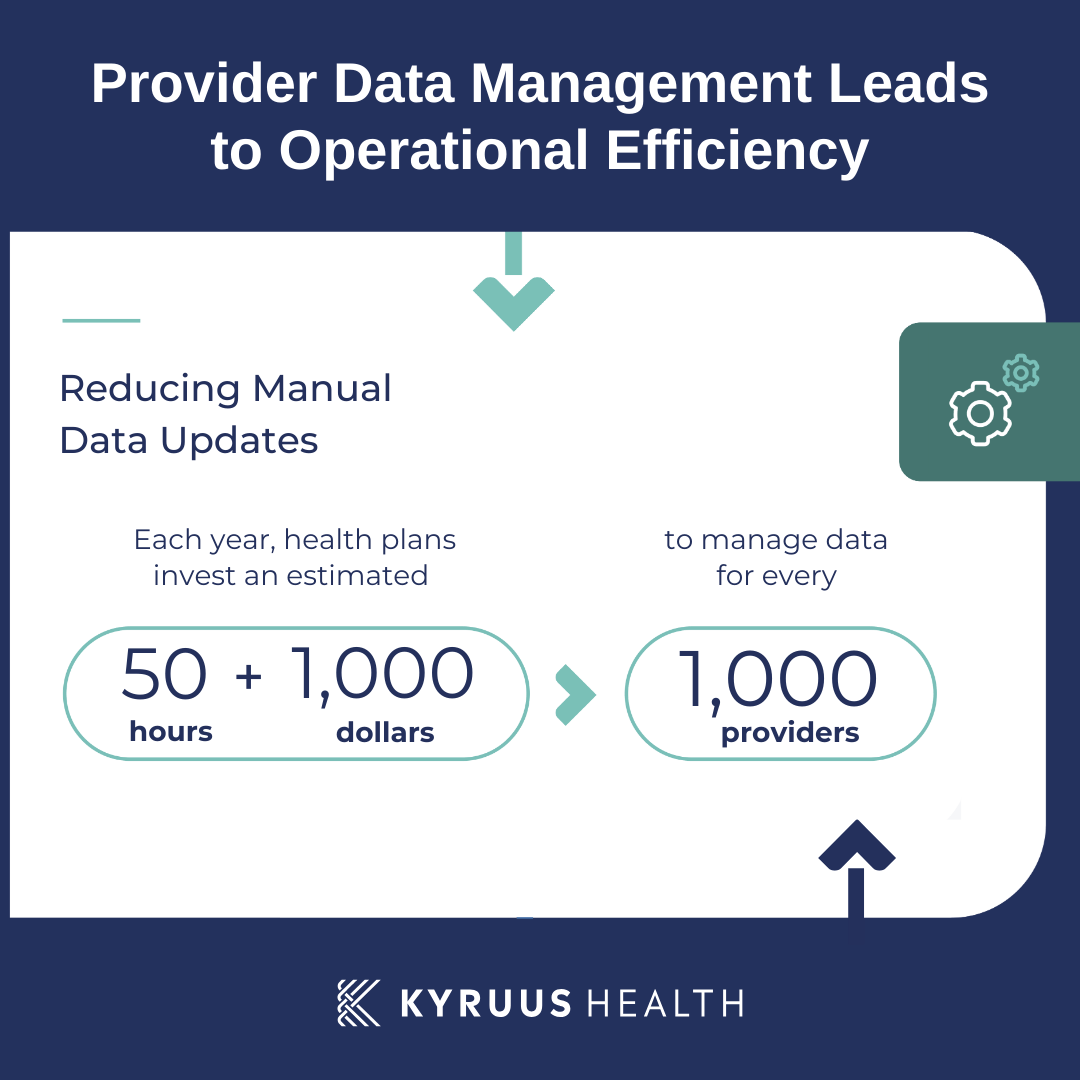 Managing provider data is a resource-intensive process, often requiring substantial time and labor for manual updates. Health plans that rely on outdated or inefficient systems for managing provider information may find themselves constantly struggling to keep up with changes, leading to higher administrative costs and operational inefficiencies.
Managing provider data is a resource-intensive process, often requiring substantial time and labor for manual updates. Health plans that rely on outdated or inefficient systems for managing provider information may find themselves constantly struggling to keep up with changes, leading to higher administrative costs and operational inefficiencies.
A centralized data management system, supported by automated workflows, can significantly reduce the burden of manual data updates. Such a system ensures that updates are reflected consistently across all channels, from member-facing directories to internal systems used by customer service agents. This not only improves the accuracy of provider data but also enhances operational efficiency, freeing up resources that can be redirected toward more strategic initiatives.
Key Strategies for Effective Provider Data Management
To successfully manage provider data and realize the benefits outlined above, health plans should consider implementing the following strategies:
- Centralize Provider Data: Establish a centralized data repository to maintain uniformity and accuracy across all channels.
- Regular Verification: Implement regular verification processes to ensure provider information is current and compliant.
- Enhanced Provider Profiles: Offer detailed, up-to-date provider profiles that meet member expectations for comprehensive information.
- Provider-Friendly Tools: Develop tools that allow providers to easily update their own information, ensuring accuracy and reducing administrative burdens.
- Online Scheduling: Integrate online scheduling functionality to improve access to care and reduce out-of-network claims.
- Automated Data Management: Leverage advanced technologies to automate data management processes, enhancing efficiency and reducing costs.
Conclusion: Why Provider Data Management is a Business Imperative
Effective provider data management is no longer a luxury for health plans—it is a necessity. Accurate, timely, and comprehensive provider data drives improvements in member experience, access to care, compliance, provider collaboration, and operational efficiency. Health plans that prioritize provider data management will not only reduce costs and avoid penalties but also position themselves for long-term success by building trust with their members and providers.
By investing in robust provider data management solutions, health plans can unlock the full potential of their provider networks, improve member satisfaction, and drive measurable financial benefits. For those ready to take the next step, Kyruus Health offers innovative provider data management solutions designed to meet the unique needs of health plans and deliver a clear return on investment. Contact us today to learn more.



