In today’s healthcare landscape, the stakes around provider data accuracy have never been higher. For many healthcare organizations, what was once viewed as a compliance requirement is now recognized as a strategic imperative—one that underpins member and patient experience, digital engagement, and even the ability to leverage emerging AI capabilities.
In a recent panel at Becker’s Payer Issues Roundtable, featuring four leaders from payer and provider organizations, the conversation made one thing clear: getting provider data right is no longer optional. It’s fundamental to being competitive in a market where patients and members expect seamless, personalized care experiences.
The Patient and Member Experience Starts Long Before Selecting Care
More than ever, people are shopping around for care before selecting a provider. Holly Sullivan, VP of Brand, Marketing, and Consumer Experience at Corewell Health, shared that 65% of prospective patients bypass their site altogether, coming through third-party platforms and search engines to evaluate networks and providers. If the data on those external platforms is inaccurate or incomplete, both providers and payers risk losing business before the funnel even starts.
That insight has sparked a shift in strategy—organizations are investing in enriched provider profiles that reflect not only specialty and location but also photos, languages spoken, credentials, and scheduling availability. These enhancements don’t just improve visibility; they help build trust and connection in the digital discovery phase.
The Provider Data Ripple Effect
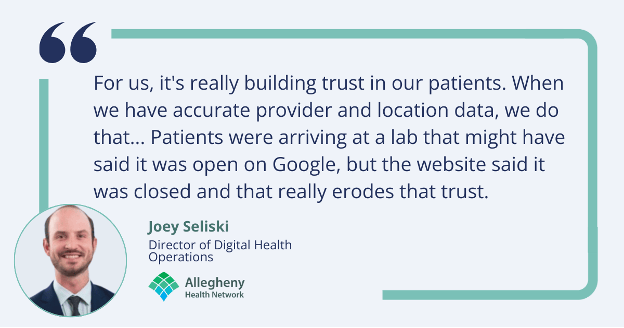
For health plans and providers alike, inaccurate or inconsistent provider data creates friction across nearly every touchpoint:
- Digital tools surface conflicting results, confusing patients and members.
- Directories may be out of sync with operational realities, leading to misrouted appointments or dissatisfaction.
- Call centers struggle to answer basic questions about in-network status and cost.
But, when provider data is accurate and unified across systems, the ripple effect is powerful: patients and members find the right doctors faster, frontline staff are better equipped, and digital tools deliver on their promise of ease and clarity.
AI Readiness Begins with Data Readiness
All four panelists agreed: if you want to unlock the potential of AI, start by getting your provider data house in order. Organizations are already using AI and machine learning to:
- Validate provider entries against external sources.
- Auto-generate bios from resumes.
- Proactively recommend care based on individual gaps and preferences.
- Power smart scheduling and virtual assistants that respond to questions like “Who’s in my network?” or “What’s the cost of this visit?”
And yet, all of these use cases rely on one thing—connected, current, and comprehensive provider data. Without that, even the most advanced AI models will underperform or deliver the wrong experience.
From Compliance Burden to Strategic Opportunity
Much of the progress happening today is because leaders are rethinking how their organizations govern provider data. Rather than treating it as a siloed function, teams are forming cross-functional governance groups that include stakeholders from operations, IT, marketing, call centers, and medical staff. These groups meet regularly to align on how provider information is collected, ranked, displayed, and updated.
The results? Less friction, more consistency, and faster responses to market needs.
However, friction does remain—particularly when it comes to how different types of providers (employed, affiliated, independent) are ranked in search results. These discussions can get “spicy,” as one panelist joked, but they’re essential to creating a search experience that is both equitable and transparent.
A Look at National Data Efforts
When asked about the promise of a centralized, national provider directory, panelists acknowledged efforts like CMS’s push to make the National Plan and Provider Enumeration System (NPPES) the single source of truth. But challenges remain: many providers still don’t understand how or when to update their information in NPPES, and health plans often find their own data to be more accurate.
That hasn’t stopped teams from using NPPES as a benchmark—they regularly download the data and compare it to their internal records to identify gaps and areas for improvement. But for now, it’s supplemental—not a replacement for their own provider data strategies.
The Path Forward
The message from the panel was clear: if we want to create a healthcare system that’s digitally enabled, consumer-centered, and AI-ready, we must begin with provider data. That means treating it not as an IT problem or a compliance checkbox, but as a strategic pillar that touches every corner of the organization.
Health plans and providers who embrace this mindset will not only deliver better experiences—they’ll be ready for whatever comes next.