REAL Health Providers Act: Proposed MA Plan Provider Directory Requirements
It can be difficult for health plans to keep track of the compliance requirements around maintaining accurate provider directories. Provider data accuracy requirements are constantly evolving and health plans need to verify that their directories don’t have outdated information. Kyruus Health monitors legislation that may impact health plans with respect to our care access platform, and the recently proposed REAL Health Providers Act falls into that category.
Kyruus Health’s Vice President of Regulatory, Sydney Edwards, breaks down the bipartisan legislative proposal formally called the Requiring Enhanced and Accurate Lists (REAL) of Health Providers Act. She summarizes the provider directory requirements that Medicare Advantage (MA) plans would need to meet, and explains how meeting them helps avoid ghost networks—illustrating the importance of provider data accuracy to health plans and their members. For a transcript of the video, continue reading.
Requiring Enhanced and Accurate Lists (REAL) Health Providers Act
We’ve had a lot of questions about the proposed bipartisan legislation called the REAL Health Providers Act. It was introduced to ensure Medicare Advantage (MA) plans maintain accurate provider directories and protect consumers from unexpected health care costs. I’m going to review the key provisions so you have an understanding of how it might impact your business.
While these requirements are specific to Medicare Advantage plans, the underlying problem of inaccurate provider data is universal. Imagine a member’s frustration when searching for care, only to find the provider has outdated contact information, or is not accepting new patients or even worse, is no longer in-network. These “ghost networks” occur in directories where providers seem readily available, but in reality are not. This pervasive issue is what the REAL Act attempts to address.

Key Requirements of the REAL Health Providers Act
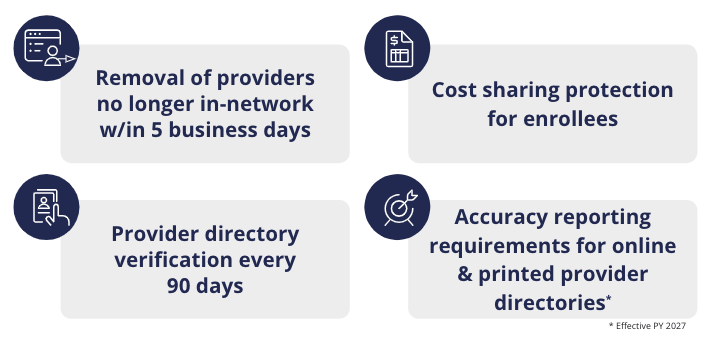
If passed, beginning plan year (PY) 2026, the REAL act would require:
-
Removal of providers no longer in-network within 5 business days
- From both online and print directories after determining the provider is no longer participating in the Medicare Advantage network.
-
Cost sharing protections for enrollees
- For services resulting from incorrect provider network information – so members don’t get stuck with out-of-network charges due to bad information.
- As well as member notification of cost sharing requirements – during enrollment, within EOBs as well as within the directory itself – creating transparency for members.
-
Provider directory verification every 90 days
- Also called attestation, to ensure provider information is correct.
- For unverified providers, the ability to indicate in the directory that information displayed may not be up-to-date.
-
Accuracy reporting requirements for online & printed provider directories
- An accuracy score will be published annually on CMS’s website in MRF format. More guidance is expected to come on how to measure and report the score.
- CMS will pay particular attention to data accuracy for mental health and substance use disorder providers.
Provider Data Accuracy and Care Access
Provider data accuracy is at the core of our mission to connect people to the right care. Strengthening requirements for Medicare Advantage plans to maintain and update accurate information is important to building member trust, maintaining satisfaction, and streamlining access to care—particularly for specialties with historically high inaccuracy rates.


